Penile Cancer
Penile cancer is an uncommon malignancy that is more frequently reported in elderly males. The pathophysiology revolves around malignant transformation of penis surface cells (also referred to as squamous cells); thereby leading to malignant growth or mass formation. In very rare cases, glandular cells of sweat glands may undergo malignant changes to form a lump. The histological type of penile cancer can only be determined after biopsy and examination.
According to latest estimates, approximately 1820 new cases of penile cancer will be diagnosed in the year 2015 (1). Fortunately, early diagnosis and timely management of penile cancer is associated with good prognosis. Based on the latest estimates of the American Cancer Society, penile cancer is expected to claim approximately 310 deaths in the year 2015.
What Else Should You know About Penile Cancer?
 The incidence of penile cancer is fairly low in United States (less than 1 case per 100,000 of the general population). However, in other parts of the world (especially Africa and South American communities), penile cancer accounts for 10% of all the reported cases of cancer. In United States, penile cancer accounts for less than 1% of all the reported malignancies.
The incidence of penile cancer is fairly low in United States (less than 1 case per 100,000 of the general population). However, in other parts of the world (especially Africa and South American communities), penile cancer accounts for 10% of all the reported cases of cancer. In United States, penile cancer accounts for less than 1% of all the reported malignancies.
There are several risk factors that may aggravate the risk of developing penile cancer; such as:
- Advancing age (incidence is fairly high in males after the age of 60 years)
- History of multiple sex partners
- Positive history of chronic tobacco or drug abuse
- Certain congenital or acquired anatomical defects such as phimosis
- HPV (Human papillomavirus) infection is also associated with a higher risk of penile cancer
- Poor genital hygiene (data indicates that uncircumcised males are more likely to develop penile cancer)
Classic Symptoms of Penile Cancer
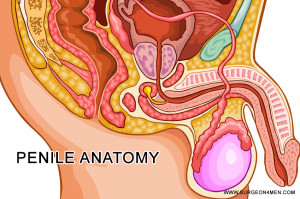
Following sign and symptoms suggest a penile malignancy. It is imperative to keep in mind that the malignant lesions of penis are usually concealed and are only visualized once the prepuce (or foreskin) is completely removed. Most characteristic sign and symptoms include:
- Redness, rash or irritation of the skin of penis
- Appearance of sores or lumps on the surface of penis
- Smelly discharge or bleeding from the penis
- Abnormal changes in the color or appearance of the foreskin
- Swelling or edema of the distal end of penis
- In some advanced cases of penile cancer, the malignant cells may spread to draining lymph nodes, leading to lymph adenopathy (or enlargement of groin lymph nodes)
Experts suggest that onset of a painless lesion or mass on the penis that does not solve or improve over a period of 4 – 6 weeks should be suspected as a malignant lesion.
 How Is Penile Cancer Diagnosed?
How Is Penile Cancer Diagnosed?
Besides history taking and clinical examination, several clinical tests are also conducted to confirm the diagnosis of penile malignancy. Most reliable and sensitive diagnostic modalities are:
- Ultrasound: Ultrasound is performed to ascertain the site, size and consistency of the malignant lesion and in order to differentiate it from other inflammatory or infectious conditions.
- Biopsy: Biopsy is the gold-standard of penile cancer diagnosis. It involves sampling of a small portion of the tissue to detect the presence of malignant cell under a microscope.
How to Manage or Treat Penile Cancer?
Once the diagnosis is confirmed, several palliative or curative surgical procedures can be adopted to get rid of cancer mass. Most frequently used modalities of care in penile cancer management are:
- Surgery
- Radiation therapy
- Chemotherapy
- Biologic therapy
- Radio sensitizers
Almost all treatment modalities of penile cancer are associated with varying degrees of erectile dysfunction and other sexual/ reproductive complications.
References:
- http://www.cancer.org/cancer/penilecancer/detailedguide/penile-cancer-key-statistics
- Inman, B. A., Stewart, S. B., & Kattan, M. W. (2013). Staging and Risk Stratification in Penile Cancer. In Penile Cancer (pp. 11-42). Humana Press.
- Ficarra, V., Zattoni, F., Artibani, W., Fandella, A., Martignoni, G., Novara, G., … & Members, G. P. C. P. (2006). Nomogram predictive of pathological inguinal lymph node involvement in patients with squamous cell carcinoma of the penis. The Journal of urology, 175(5), 1700-1705.
- Bleeker, M. C., Heideman, D. A., Snijders, P. J., Horenblas, S., & Meijer, C. J. (2012). Epidemiology and Etiology of Penile Cancer. In Textbook of Penile Cancer (pp. 1-11). Springer London.