Diagnosis of Prostate Cancer
Early identification and prompt management can greatly reduce the morbidity and mortality associated with prostate cancer. For example, according to the data reported by in the peer reviewed journal European Urology (1), population-based cancer screening trial of Gothenburg has resulted in the reduction of mortality associated with prostate cancer by 44%.
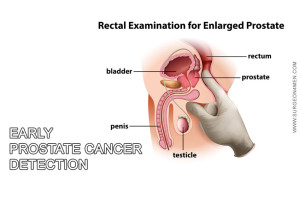
However, investigators strongly believes that tests like PSA and digital rectal examination are not sufficient to make the diagnosis of prostate cancer. Therefore, the current gold standard test for the detection and confirmatory diagnosis of prostate cancer is ultrasound-guided biopsy (which should be ideally performed under local anesthesia).
I. Trans-rectal Ultrasound
Trans-rectal ultrasound is a test that is conventionally performed to get more detailed information about the size, consistency and texture of prostate tumor or enlargement. The test is performed by inserting a probe into the rectum (after lubrication) to assess the local environment in order to devise a more comprehensive diagnostic regimen.
Trans-rectal Ultrasound procedure is non-invasive and usually painless (although a little embarrassing for the patient) and can be performed as an out-patient procedure in under 10 minutes. Other applications of this test are in; detection of PSA density, cryosurgery and radiation therapy (or brachytherapy).
II. Ultrasound-guided Prostate Biopsy
 Although, more than 90% cases of prostate cancer are detected by screening in the United States (via PSA test); the prognosis and response to therapy is greatly dependent on the accurate diagnosis; which includes staging, grading and aggressiveness of tumor (2). Obviously this is only possible if your healthcare professional performs histological examination after obtaining a tissue biopsy of the tumor.
Although, more than 90% cases of prostate cancer are detected by screening in the United States (via PSA test); the prognosis and response to therapy is greatly dependent on the accurate diagnosis; which includes staging, grading and aggressiveness of tumor (2). Obviously this is only possible if your healthcare professional performs histological examination after obtaining a tissue biopsy of the tumor.
Ultrasound-guided core-needle prostate biopsy is performed by introducing a fine needle in the prostatic tumor to take approximately 8 to 12 tissue samples under local anesthesia. The procedure is usually painless and can be performed as an out-patient procedure within 10-15 minutes. After histopathological evaluation, doctor’s advice if the tumor is differentiated (associated with good prognosis) or undifferentiated (associated with a bad prognosis).
Although, the sensitivity and specificity of Ultrasound-guided core-needle prostate biopsy is fairly high (mainly due to multiple sampling technique); it is possible in about 5 -15% cases to miss the cancerous tissue. In all such cases, a repeat biopsy is usually recommended.
Other tests that are also performed to diagnose the prostate cancer are:
III. Gleason Score for Grading
This test is primarily used to detect the aggressiveness or localized spread of prostate cancer. In this test, investigators score the prostate cancer on the basis of histological and pathological characteristics from 1 to 10. A lower Gleason score (6 or less) is associated with good prognosis and tumor cells are well-differentiated. A higher Gleason score (8 to 10) is suggestive of aggressive poorly-differentiated cancer that is associated with a worse prognosis.
IV. Tests for Staging
Staging refers to localized or distant spread of cancer cells. Most common sites of prostate metastasis are; bone, liver and brain. It is imperative to mention that staging of cancer is very important before initiating the therapy and establishing prognosis.
Following tests are generally performed to ascertain the stage of prostate cancer:
- Bone scan: To detect bone and spine metastasis.
- Ultrasound: Depending upon the symptomatology and pattern of spread, your doctor may advice ultrasound of liver, lungs and other vital organs to check for metastatic seeding.
- Computerized tomography (CT) scan: CT scan detects the distant metastasis as well as local spread to major vessels/ lymphatics and nerves.
Other tests includes; Positron emission tomography (PET) scan and Magnetic resonance imaging (MRI).
Staging and Grading of Prostate Cancer
Based on the tests and staging modalities discussed above, prostate cancer can be classified into 4 primary stages; these are:
- Stage 1: Localized disease with an overall small sized tumor and well-differentiated cancer cells.
- Stage 2: The size of the cancer may still be small but there is a high propensity of involvement of both sides of prostate.
- Stage 3: Spread of prostate malignancy to the surrounding tissue is classified under stage 3. Most common sites if early spread are seminal vesicles and nearby tissues.
- Stage 4: Distant spread to vital organs via lymphatic or vascular spread. Most common sites are; lungs, urinary bladder, brain, distant lymph nodes and bones.
Depending upon the diagnosis, further course of action is planned. For non-problematic localized small tumors, no active intervention is planned.
References
1. Heidenreich, A., Bellmunt, J., Bolla, M., Joniau, S., Mason, M., Matveev, V., … & Zattoni, F. (2011). EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. European urology, 59(1), 61-71.
2. Hoffman, R. M. (2011). Screening for prostate cancer. New England Journal of Medicine, 365(21), 2013-2019.
3. Cheng, L., Montironi, R., Bostwick, D. G., Lopez‐Beltran, A., & Berney, D. M. (2012). Staging of prostate cancer. Histopathology, 60(1), 87-117.
4. Heidenreich, A., Bellmunt, J., Bolla, M., Joniau, S., Mason, M., Matveev, V., … & Zattoni, F. (2011). EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. European urology, 59(1), 61-71.